Pisgah Legal Services supports the work
of the NC Medicaid Ombudsman.
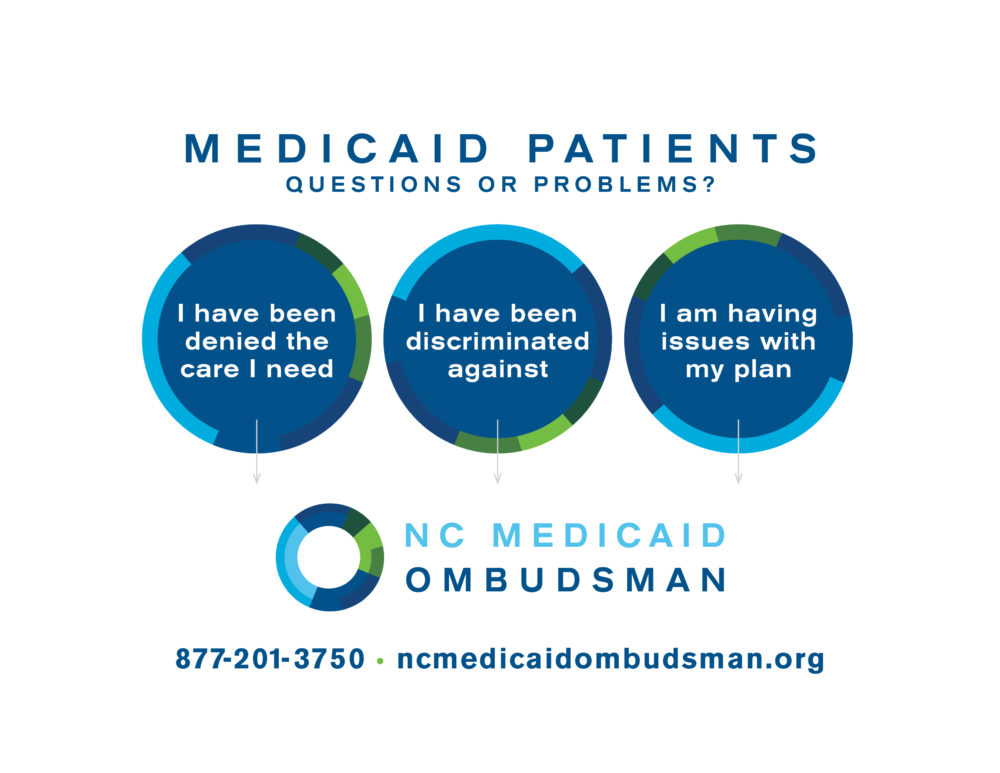
What is the NC Medicaid Ombudsman?

The NC Medicaid Ombudsman is a free, confidential service that can answer your questions about Medicaid Managed Care, and help you solve problems with your coverage and care.
The NC Medicaid Ombudsman can tell you your rights under Medicaid Managed Care, and refer you to a legal aid organization if your rights are being denied.
They also connect people to resources like legal aid, social services, housing resources, food assistance and other programs.
The Ombudsman can help you get the care you need, if:
- You are denied the care you need
- Your health plan won’t cover services you need
- It takes too long to get the care you need
- You have to travel too far
- You can’t get transportation
- You need services for mental health or an intellectual or developmental disability
The Ombudsman can help you change what care you can access, if:
- You have problems changing to a different health plan
- You have problems changing your primary care provider
The Ombudsman can help you with barriers to care and coverage, if:
- You can’t access material or information in your preferred language
- You feel a health plan, provider or enrollment representative has discriminated against you
Medicaid Managed Care – a big change for many with Medicaid
If you depend on North Carolina Medicaid, the way you receive health care from your doctors and health care providers may have changed. The State has transitioned most Medicaid recipients to Medicaid Managed Care to provide you with care that addresses your health needs and reduces the high cost of health care.
What about Medicaid Direct?
People who have serious mental illness or developmental disabilities, people who have Medicare coverage, people in a Medicaid waiver program and some others do not have to move to a Medicaid Managed Care health plan just yet.
The transition to Medicaid Managed Care is complicated. Your unique health care situation includes different doctors, nurses, therapists and services like transportation that should work together.
When you cannot get clear information about what is changing, why it’s changing or what you need to do, it’s frustrating. When you are discriminated against, or are denied things like transportation or service in the language you prefer, it’s wrong.
You have rights, and the NC Medicaid Ombudsman can help!
Health plans – how they work, what to do if they don’t
Before July 1, 2021, you could work directly with your doctor (or pharmacist) to know if they accepted NC Medicaid for check-ups and other services (or prescriptions). You could also check with Medicaid to learn about other services or where to go for a medical emergency.
With Medicaid Managed Care, most Medicaid recipients now have health plans managed by private companies that work with specific doctors and may offer additional services. Not all doctors work with all health plans and some require your doctor to check with them before approving a service
It is up to you to understand which doctors and services are covered as part of your health plan. Your doctor’s office may not be familiar with your health plan or what is or is covered, so it is best to communicate with someone at your health plan directly.
If your health plan is not helpful, or you are still confused about which doctors and services are covered, the NC Medicaid Ombudsman can help!
You can change your health plan for up to 90 days after the start date shown on your health plan enrollment letter. After 90 days, you must wait until your next recertification date to change your health plan unless you have a special reason.
If you need help changing your plan, the NC Medicaid Ombudsman can help.
